Think about you’re a clinician at a well being system, understanding that your database is full of related scientific insights. You recognize this information could be extremely useful in navigating the nuances of every affected person case, as there may very well be pertinent data that influences the therapy path you prescribe.
The problem is which you could’t at all times entry this information or make it actionable, and when you can it’s not prone to be inside a related scientific timeframe. In different phrases, you will have a goldmine of knowledge that may improve affected person care, however lack the instruments to put it to use successfully.
The obstacles to accessing this information are multifaceted and largely past your management. Technical obstacles, comparable to fragmented and incompatible tech stacks, scatter information throughout numerous well being programs and care suppliers, creating silos that hinder seamless entry.
On prime of those technical challenges, you’re grappling with extra speedy, tangible constraints: hovering affected person volumes and an overburdened workforce. These pressures exacerbate the wrestle, leaving you and your care workforce overwhelmed and unable to harness the information’s energy to boost affected person outcomes.
Technological developments have revolutionized healthcare, making as soon as sci-fi-like improvements like robotic surgical procedures, telemedicine, genomic medication and superior imaging a actuality. These instruments have simplified procedures and improved outcomes considerably.
Nonetheless, regardless of these exceptional developments, I used to be greatly surprised upon rereading a research carried out by Johns Hopkins quantifying the devastating impression of misdiagnosis, which is way extra staggering than I had imagined. Would you consider me if I stated that as much as 795,000 deaths and severe medical harms (i.e. everlasting incapacity) annually are a results of medical error within the U.S.? This might make misdiagnosis a number one reason for dying, surpassing coronary heart illness, most cancers and accidents.
That introduced me to this query: May enhancing entry to information assist flip the tides?
The Untapped Knowledge Mine
Take into consideration the well being system as a mining website. Extra particularly, a mine known as a “vertical shaft single stage hoisting mine.” (Sounds fancy, proper?) Image it: arduous hats, pickaxes and possibly even a canary or two. See the diagram beneath of such a mine for context and its healthcare operation equal (with AI):
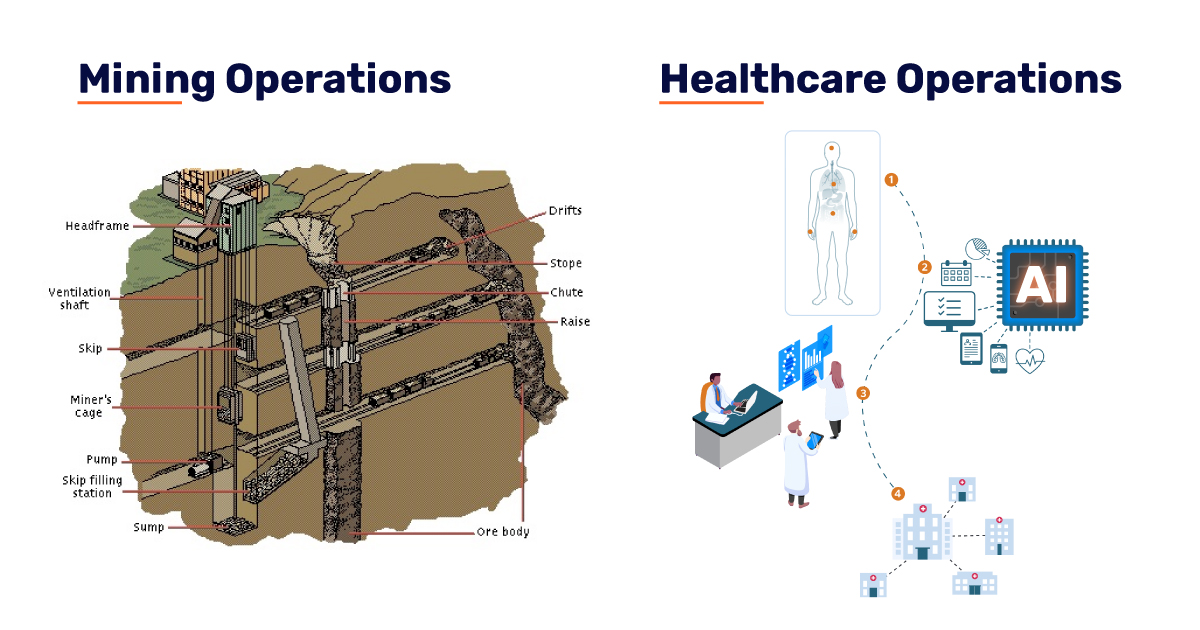
Now take into consideration the mining operation as a healthcare community. Sitting above floor within the headframe are the operational and administrative items, together with a lot of the employees. Right here you will have your administrative employees, your tech stack, clinicians and even your sufferers. Every part is accessible, inside attain and working easily. Now you enter the proverbial miner’s cage and work your method underground. That is the place you discover issues like EHRs, the imaging division and different specialists and proceduralists, all using what’s out there to them to achieve deeper insights into affected person circumstances and supply optimum care. The ore our bodies (all the way in which on the backside) are the information. We all know that in in the present day’s digital age, there’s an amassing of knowledge in well being programs.
To place the amount of knowledge into perspective, a projection from the World Financial Discussion board states that the quantity of knowledge that’s being created in healthcare “is nearly incomprehensible,” globally producing 2.3 zettabytes of knowledge – or 2.3 trillion DVDs (keep in mind these?) price of knowledge.The issue is that as suppliers and sufferers navigate the advanced healthcare panorama, making quite a few stops alongside the way in which to obtain care, they miss important alternatives to succeed in the true worth of their information.
Actually, it’s estimated that 97% of this information goes unused.
With such an amazing quantity of knowledge being generated, it’s no marvel that a few of these priceless insights typically slip by the cracks. However what if there was a option to harness this data successfully? That is the place AI steps in, providing a robust answer to mine healthcare information and uncover new alternatives for improved care inside well being programs.
How Does AI Work because the Pickaxe?
My proposition is that AI platforms act because the pickaxe that may make this stockpile of knowledge accessible to clinicians and, thus, actionable. This might lead to remodeling care paths and, subsequently, affected person outcomes.
When correctly chosen and carried out, an AI platform can:
- Scale Throughout the Total Well being System: AI’s capability to combine in numerous departments and programs makes it scalable, making certain constant and complete information evaluation and perception technology.
- Course of Knowledge in Actual Time: AI can analyze huge swaths of knowledge in actual time, offering clinicians with up-to-the-minute insights that may instantly affect therapy choices. This real-time processing is essential in emergency and important care settings, the place well timed choices can impression outcomes.
- Analyze a Broad Spectrum of Knowledge: AI doesn’t restrict itself to a single information sort, of which there are many. It might probably combine and analyze EMRs, lab outcomes, imaging research, vitals and even patient-reported outcomes. This complete strategy ensures that no related data is missed.
- Help Customized Medication: By analyzing particular person affected person information alongside huge datasets, AI can tailor remedies to every affected person’s distinctive wants, transferring away from a one-size-fits-all strategy to additional personalize care.
- Improve Operational Effectivity: AI can streamline administrative duties, optimize useful resource allocation and scale back redundancies, enhancing the effectivity of care supply.
Think about a case research involving grownup oncology sufferers, the place AI was used to prioritize the detection of incidental pulmonary embolism (iPE) on routine chest CT scans. On this research, AI was evaluated alongside historic controls and potential evaluation. Throughout three distinct durations, the AI demonstrated exceptional effectiveness: it detected 91.6% of true-positive circumstances with a specificity of 99.7%, decreasing the median detection and notification time from 7,714 minutes (routine workflow) to simply 87 minutes. Moreover, the radiologists’ missed price of iPE plummeted from 44.8% with out AI help to a mere 2.6% with the AI software. This important discount in missed circumstances and expedited prognosis highlights how AI can uncover vital care alternatives that busy physicians would possibly overlook, in the end resulting in sooner, extra correct therapy paths for sufferers. Moreover, these types of findings may unearth future care alternatives.
Carried out on a large scale, this type of technological shift in well being programs would sign a metamorphosis in care supply, exhibiting the impression for AI in real-time scientific environments. It’s not nearly mining the information; it’s about revolutionizing the way in which healthcare suppliers work together with and make the most of this information, resulting in improved affected person outcomes and extra environment friendly healthcare programs.